Public Health
Tuberculosis: An Ancient and Ongoing Epidemic
Tuberculosis (TB) is an airborne infectious disease occurring since ancient times. Many people including celebrities in history such as John Harvard and Lu Xun (鲁迅) died from TB. The cause of this disease was not known until 24 March 1882 when German bacteriologist Robert Koch announced the discovery of the TB bacterium, Mycobacterium tuberculosis. Commemorating such an important discovery, the date 24 March is recognized as World TB Day which becomes an annual event to raise public awareness about TB in order to prevent and control the disease effectively and proactively.
Despite advances in diagnosis and treatment technologies, TB remains a global pandemic. The World Health Organization (WHO) declared TB a public health emergency in 1993.
There were estimated 10 million people fell ill with TB and 1.5 million died from the disease worldwide in 2018. Eight countries accounted for about two thirds of the total, with India leading the count, followed by China. The prevalence of TB in Hong Kong is steady at 4,000 to 5,000 cases per year; however, such incidence rate with respect to population is still significantly higher than those in many developed countries including Japan, UK and US (Table below). Within HKUST, less than one TB incidence was recorded per year with the most recent case arose in November 2019.

Table of Global, National and Local Statistics on TB in Recent Years
| 2018 | Worldwide | India | China | Hong Kong | Singapore | Japan | UK | US |
| Population in 2018 (million) | 7,604 | 1,353 | 1,428 | 7 | 6 | 127 | 67 | 327 |
| Total TB incidence in 2018 | 10,000,000 | 2,690,000 | 866,000 | 4,900 | 2,700 | 18,000 | 5,400 | 9,800 |
| Total TB incidence rate in 2018 (per 100,000 population) | 132 | 199 | 61 | 67 | 47 | 14 | 8 | 3 |
TB Factsheet
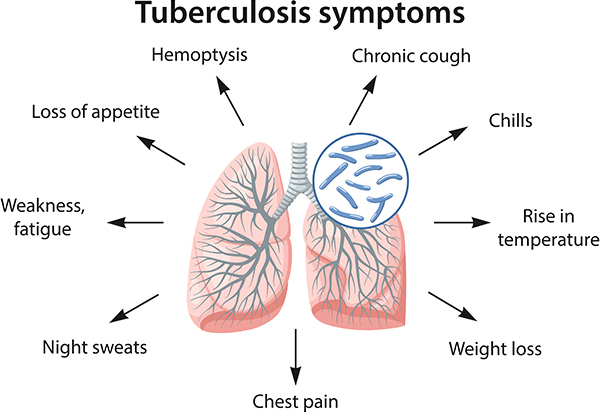
| Types; Symptoms | TB usually affects the lungs (pulmonary), but it can also affect other parts of the body including lymph nodes, bones, joints, vertebral spine, brain and kidney (extrapulmonary). The symptoms include persistent cough, blood-stained sputum, loss of body weight, afternoon fever and night sweating. Depending on the parts of the body being affected, other symptoms may also occur. Pulmonary TB can be contagious whereas extrapulmonary TB is usually not contagious according to the Centers for Disease Control and Prevention (CDC) of the US. |
| Latent Period; Progression from Infection to Disease |
The latent period of TB varies from weeks to decades depending on individual risk factors including personal immunity. Within weeks of being infected with the tubercle bacilli, a primary infection will be developed in the lungs of the infected individual. The great majority of infected people will not fall ill and experience no symptoms, in which case it is known as latent TB infection. Although latent TB may persist, it is not contagious. However, a small proportion of the infected people, 5% to 10%, will go on to develop active TB disease, which is contagious, at some stages in their lives. |
| Transmission | TB can be spread through air. When the infected person coughs or sneezes, the Mycobacterium tuberculosis gets into the air and this can result in infection if a susceptible person is in contact for a prolonged duration. People with active pulmonary TB disease are most likely to spread it to the others they spend time with frequently, i.e. their close contacts, including family members, friends, co-workers and school mates. However, TB is not spread by shaking hands, sharing food or drink, touching bed linens or toilet seats, sharing toothbrushes or kissing according to CDC. |
| Vulnerable Groups | People who have been recently infected with Mycobacterium tuberculosis and with medical conditions that weaken the immune system are at higher risks for developing active TB disease. According to WHO, the probability of developing active TB disease is much higher among people affected by risk factors such as human immunodeficiency viruses (HIV), undernutrition, diabetes, smoking and alcohol consumption. |
| Diagnosis | The common tests to diagnose TB include chest x-ray examination, sputum smear microscopy, sputum culture methods, Mantoux tuberculin skin test and blood tests. Other technologies, such as computerized tomography (CT), bronchoscopy and lung biopsy, and newly developed skin tests including C‐Tb test and Diaskin test, may also be used for diagnosis. |
| Treatment | Effective drug treatments were first developed in the 1940s. The treatment recommended by WHO for cases of drug-susceptible TB disease is a 6-month regimen of four first-line drugs: isoniazid, rifampicin, ethambutol and pyrazinamide. Treatment success rates of at least 85% for cases of drug-susceptible TB are regularly reported to WHO by its 194 Member States. Treatment for people with multidrug-resistant TB or rifampicin resistant TB (MDR/RR-TB) is longer and requires drugs which are more expensive and more toxic. The latest data reported to WHO show a treatment success rate for MDR-TB of 56% globally. Effective treatment of infectious patients is the most important component for TB control. The use of directly observed treatment, short course (DOTS) is strongly recommended by WHO in the control of TB. |
| Regulations in HK | TB is one of the 51 notifiable infectious diseases in accordance with the Prevention and Control of Disease Ordinance (Cap.599) in Hong Kong. All registered medical practitioners are required to notify the Centre for Health Protection (CHP) all suspected or confirmed cases of TB diseases using the specific notification Form. |
| Control Programme in HK; Vaccination | In Hong Kong, the core components of the local TB control programme include case finding, effective chemotherapy, treatment of latent TB infection, Bacillus Calmette-Guerin (BCG) vaccination and health education. The Tuberculosis & Chest Service, Department of Health provides BCG vaccination to all newborns in Hong Kong to protect them against TB. Children residing in Hong Kong, who are aged below 15 and have never received BCG before, are also advised by CHP to receive the vaccine. |
| Prevention |
Prompt Response to suspected or confirmed TB cases:
Maintain good personal hygiene:
Travel health advice:
|
| Links |
Timeline - Response to a TB Case in the HKUST
| Date | Start of case in Nov 2019 |
| 21 Nov 2019 |
|
| 25 Nov 2019 |
|
| 26 Nov 2019 |
|
| 27 Nov 2019 |
|
| 29 Nov 2019 |
|
| 05 Dec 2019 |
|
| 06 Dec 2019 |
|
| 19 Dec 2019 |
|
| 31 Dec 2019 |
|
| 02 to 09 Jan 2020 |
|
| Close of case in Jan 2020 | |
| Abbreviations: Health, Safety and Environment Office (HSEO) Office of the Dean of Science (DSCI) Student Housing and Residential Life Office, Dean of Students' Office (SHRLO, DSTO) |
|
